Summit on Biologics and Biosimilars Tackles Choice, Switching & Patient Access
April 10, 2017
Physicians and patients are no longer asking if a biological medicine is the best choice, but – more likely – which biological medicine is the best choice. This opening thought from Alliance for Patient Access Chairman David Charles, MD, set the tone for the organization’s second annual National Policy and Advocacy Summit on Biologics and Biosimilars, held Thursday in Washington, DC.
Patients, government representatives, physicians and advocates explored throughout the day-long event how more biological options present both new challenges and new possibilities for treatment. The event was co-sponsored by the Institute for Patient Access and the Biologics Prescribers Collaborative.
Policy & Advocacy Issues
The summit’s policy discussion spanned both global and U.S. issues.
Global Issues
An international panel examined Europe and Latin America’s experiences with biologics and biosimilars, including what lessons they might offer the United States.

- Patient advocate Neil Betteridge of the UK described how “clandestine” switching of patients from a biologic to a biosimilar in Denmark had damaged trust between physicians and their patients. He also conveyed findings by Professor Michael Kaeding of the University of Duisburg-Essen that patients’ adverse events were underreported. “Physicians and patients need to be better informed about tracking and monitoring…” he emphasized.
- Patient advocate Eva Maria Ruiz de Castilla described the patchwork regulatory approval process in Latin America and the complications it poses for patients and providers. She also described the region’s approach to biosimilar switching as “a matter of budget.” She emphasized the need for advocates to push for a more patient-focused approach.
- Oncologist Arturo Loaiza-Bonilla, M.D., gave the physician’s perspective on indication extrapolation. He pointed to rituximab for cancer patients as an example of why extrapolating approved uses for a biologic that treats multiple conditions can be problematic. “The impact of a drug on immune systems differs across disease state,” he noted.
Panelists pointed to work by the Global Alliance for Patient Access to illustrate how coordinated advocacy is encouraging informed policymaking on the international stage.
U.S. Issues
Questions of switching resurfaced in the “Policy Advocacy in the States” panel, which also examined the problems associated with step therapy:
- Kevin Daley of the Coalition of State Rheumatology Organizations described patients’ frustrations with non-medical switching after spending “six months to a year” working with their doctor to pinpoint the right medication. He called it “a farce” for health plans to expect savings when they wind up spending more to address the medical effects of switching.
- Kathleen Arntsen of the Lupus and Allied Diseases Association described patients’ work to get step therapy protections unanimously passed by the New York legislature. Kathleen also opened up about her personal experience with step therapy; her health plan required her to take eye drops that she couldn’t tolerate and ultimately left her without sight in one eye.
- Harry Gewanter, MD, of the Alliance for Safe Biologic Medicines offered the physician’s perspective, pointing out the irony of utilization management techniques. Health insurers are “the only people we pay to give us a hard time, to tell us no,” he explained.
Moderator Brian Kennedy used a new video from the Keep My Rx campaign to highlight state efforts to protect patients from non-medical switching.
In a morning address to summit attendees, Sen. Bill Cassidy, MD, (R-La.) provided a federal legislator’s viewpoint on breakthrough drugs’ value. A patient who benefits from a life-changing therapy such as a biologic is “working, living life, paying taxes, and not in the hospital,” Sen. Cassidy explained, adding that “If there’s a breakthrough therapy, it needs to be quickly approved.”
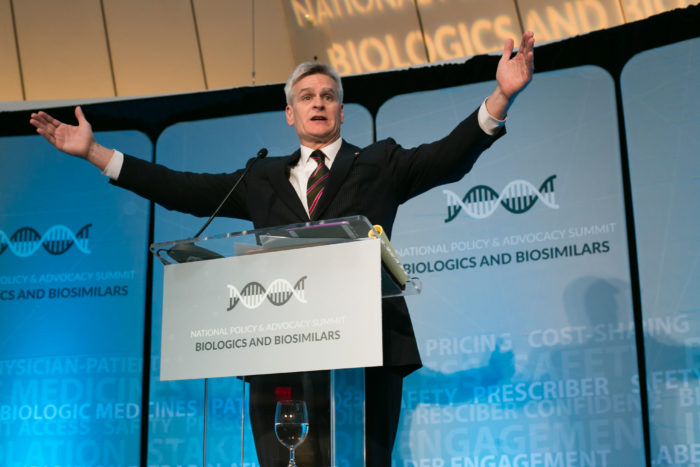
Sen. Cassidy emphasized that policymakers must determine how to advance access to breakthrough medicine “without bankrupting the country.” He argued, however, that price controls would have the opposite effect, chilling investment and hindering innovation for conditions such as Alzheimer’s.
Food and Drug Administration Guidance
Recent FDA guidance on biosimilar naming and draft guidance on interchangeability made regulatory issues a central topic for the summit. The latter is the subject of a new Alliance for Patient Access video, unveiled Thursday morning.
The FDA’s Leah Christl, PhD, elaborated on interchangeability guidance, explaining that the agency would build upon its totality of evidence approach. She also noted that the agency may require post market data for therapies whose impact leaves “residual uncertainty.”
An afternoon panel invited further discussion on regulatory issues. Hosted by Inside Health PolicyAssociate Editor Nicholas Florko, panelists considered biosimilar labeling, the impact of distinct naming and what interchangeable biosimilars might mean for patients and policy.
- Greg Schimizzi, M.D., of the Biologics Prescribers Collaborative commended the FDA’s work toward get biologic and biosimilar agents approved. He added that “It would be nice to have statements about what is and is not an appropriate substitution.”
- Stephen Marmaras of the patient advocacy group Creaky Joints highlighted patients’ concerns that health plans will use biosimilars as “an opportunity…to exploit financial gain.” He also reiterated that biosimilar savings much reach patients through lower deductibles and premiums.
- Steven Grossman, J.D., a regulatory consultant, recalled regulatory mishaps related to generic medications during the Reagan administration. Today’s FDA “doesn’t want to have that result,” he argued, “they want to do it right.” He argued that “one of the great errors of the community is expecting [biosimilar availability] to happen quickly.”
Patient Impact
Olympic medalist and cancer survivor Shannon Miller gave the event’s keynote address, a testimony to the power of the physician-patient relationship and how breakthrough medicine saves patients’ lives.

Though best known as a seven-time Olympic gold medalist and member of the United States’ 1996 “Magnificent Seven” gymnastics team, Miller is now a women’s health advocate. In describing her battle with ovarian cancer, Miller encouraged patients, “Keep fighting and take advantage of new, breakthrough therapies!”
The day ended with remarks from AfPA Executive Director Brian Kennedy.
For related materials, see:
Social media: Coverage of #BiologicsSummit
Video: The Interchangeability Promise
Video: Understanding Non-Medical Switching
Categorized in: Blog

